Cosmetic/Plastic Surgery
1. Platelet Gel Usage in Cosmetic Surgery
William Welsh, MD
Presented at the American Academy of Cosmetic Surgery – 16th Annual Scientific Meeting, New Technologies, January 2000, Orlando, FL
Platelet gel has been obtained through a perioperative technique of differential centrifugation of autologous whole blood and applied to various wound surfaces to optimize and reduce healing time. Platelets are the first cells to respond to injury. These cells contain cytokine-laden granules and ephemeral elements which, when released into the wound milieu, aid in all phases of the healing process. Vasoconstriction, chemotaxis, cell secretion, and wound remodeling are all affected by the platelet’s initial response to injury.
A clinical study was undertaken to determine the benefits of applying a concentrate of platelets to wound surfaces. Benefits were observed clinically in control of intraoperative and postoperative bleeding in one hundred consecutive facelifts which required no reintervention of the first operated hemiface following the second side operation. Only one postoperative hematoma, which resulted from an unrecognized laceration of the left facial vein, was observed. There was significant decrease in postoperative edema of the face at forty-eight hours. Looser postoperative dressings were required, increasing patient comfort. No drains were used. All sutures and/or surgical staples were removed within ninety-six hours without dehiscences. Overall healing time was shortened, and many patients were able to return to work within 5 days.
Cost benefits are realized in the shortened operative time, fewer postoperative problems and the decreased requirement for drains and elastic dressings. Autologous blood usage is significantly more cost effective and creates a greater harvest of usable product than does cryoprecipitation of autologous blood or the use of commercially prepared fibrin glues for control of bleeding. Platelet gel has the added benefit of delivering a greater concentration of platelet products important to wound healing to the injured area.
The technique has also been employed to aid healing of bone grafts, skin grafts, decubitis repair flaps, non-healing wounds and non-shear seromas.
2. Current Applications of Platelet Gels in Facial Plastic Surgery
Facial Plastic Surgery. 2002 Feb;18(1):27-33
Section of Otolaryngology, Division of Facial Plastic and Reconstructive Surgery, Yale University School of Medicine
The response of living tissue to injury is a central component in the planning of all surgical procedures. The wound-healing process is typically divided into three phases (inflammatory, proliferative, and remodeling) and is a complex process in which a multitude of cellular and humoral components interact to restore a wound defect. Platelets and their released cytokines and growth factors are pivotal in the modulation of this entire process. Although several techniques may be used to achieve hemostasis after initial injury, few initiate and actually accelerate tissue regeneration. Both platelet gel and fibrin glue are effective hemostatic agents. Platelet gels, unlike fibrin glue, have a high concentration of platelets that release the bioactive proteins and growth factors necessary to initiate and accelerate tissue repair and regeneration. In particular, two growth factors that play a major role in platelet gels are platelet-derived growth factor, a powerful chemoattractant, and transforming growth factor beta, which significantly increases and stimulates the deposition of extracellular matrix. In creating a platelet gel, autologous blood is centrifuged to produce a concentrate high in both platelets and plasma. This concentrate can be applied to wounds, providing hemostasis, adhesion, and enhanced wound healing. Recent techniques for the autologous concentrating process have been streamlined, and now platelet gels are clinically accessible to most physicians. Platelet gels have global applications in surgery and are especially useful for the soft tissue and bony reconstructions encountered in facial plastic and reconstructive surgery. In these applications, their use has been associated with a decrease in operative time, necessity for drains and pressure dressings, and incidence of complications. When applied to bony reconstruction it provides adhesion for the consolidation of cancellous bone and comminuted fracture segments.
3. Autologous Platelet Rich Plasma in Facial Plastic Surgery
Proceedings from the 8th International Symposium of Plastic Surgery, May 2002, New York, USA
Ross A. Clevens, MD
PURPOSE: The purpose of this study is to evaluate the author’s clinical experience with autologous platelet-rich plasma (platelet gel) in 250 consecutive facial plastic and reconstructive surgery cases.
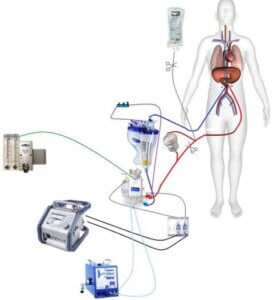
BACKGROUNG AND METHODS: Surgical applications in the current review are limited to facial procedures including aesthetic surgery (skin resurfacing, blepharoplasty, facelift, forehead lift, cervicofacial liposuction and rhinoplasty) as well as soft tissue and bony reconstructive surgery. Platelet gel is a platelet-based wound sealant or hemostatic agent that uses a high concentration of platelets and a native concentration of fibrinogen harvested by centrifugal separation of autologous whole blood. Platelet gel has characteristic components that include an array of cytokines and mediators that increase recollagenation, accelerate epidermal and epithelial regeneration, promote angiogenesis, enhance wound strength, hasten hemostasis, improve tissue regeneration , decrease dermal scarring and facilitate remodeling. Competing proprietary centrifugal systems for creating platelet gel are reviewed with respect to efficacy, cost and ease of use.
RESULTS: Autologous platelet gel significantly reduces intraoperative bleeding and oozing, minimizes bruising, decreases postoperative pain, speeds healing and hastens reepithelialization in laser skin resurfacing. Centrifugal methods achieve a 4 to 5 fold concentration in platelets and associated cytokines. Patient recovery times are reduced 25-40%. Patient acceptance levels are high.
CONCLUSIONS: Autologous platelet rich plasma is an important adjunct to accelerate healing and speed recovery in patients undergoing facial plastic and reconstructive surgery.
4. Healing Agents (Use of Platelet Rich Plasma in Facial Plastic Surgery)
Plastic Surgery Products, February 2003
Marc Kerner, MD, FACS
As we begin to understand the molecular biology of wound healing and the relationship of growth factors (proteins) and cellular mechanisms in this complex process, the methodologies to augment healing by manipulating these various factors can be applied. For years, physicians have sought to identify substances that can enhance hemostasis and promote or accelerate tissue regeneration. Autologous platelet gels (APG) are concentrations of plasma and platelets that can be directly delivered to any surgical wound.
The clinical applications of platelet gels are limited only by the physician’s imagination. We presented the first data on the use of APG as a postsurgical dressing in endonasal sinus surgery. Platelet gels have wide application in procedures involving bone or tissue grafting, as well as craniomaxillofacial applications. Marx and colleagues have published animal studies that show significant improvement in graft survival and decreased time for graft incorporation in an in vivo bone graft model. Extrapolating from this data, we have incorporated APG in virtually all of our graft procedures as well as soft tissue surgical procedures.
The primary clinical effects seen with the use of APG include a marked decrease in postsurgical swelling and bruising, decreased surgical site pain, and what appears to accelerated wound healing. We use APG in all cosmetic procedures, endoscopic brow lifts, midface lifts, lipotransfer procedures, endoscopic brow lifts, midface lifts, and laser resurfacing, in addition to any craniomaxillofacial trauma procedures and bone grafts. After applying the platelet-rich solution, we typically use the activated platelet-poor solution as an additional hemostatic agent.
Since we introduced autologous platelet gels into our clinical practice more than 3 years ago, we have virtually eliminated the need for drains, pressure dressings, and endonasal packing. I believe the cost of the disposable materials required to obtain the platelet concentrate is far less than the cost of the intangible factors of swelling, bruising, patient discomfort, and time missed from work.